Diabetes and poor sleep often go hand in hand. It's thought that diabetes may contribute to sleep loss and evidence from the Division of Sleep Medicine at Harvard Medical School points out that when you sleep poorly, it can increase your chances of getting diabetes.
Diabetes occurs when your body can't produce insulin correctly to the point where you having extra glucose levels in your blood. There are several forms of diabetes with Type 1 and Type 2 being the most common.
Diabetes and Sleep
Common connections between poor sleep and diabetes include people with diabetes often:
-
tossing and turning during the night.
-
trying to compensating their inability to sleep by consuming food in excess amounts in order to gain energy.
-
having sleep apnea and other sleep disorders in conjunction with their diabetes.
Diabetes and sleep (or lack of) was examined by researchers in a 2012 study. During the study, (published in the Journal of Sleep Research) different sleep disturbances were studied, including
-
staying asleep.
-
falling asleep.
-
getting too much sleep.
Through this study, researchers were able to link certain sleep disturbances with diabetes. The researchers claimed that you increase your risk of diabetes through sleep deprivation. However, it can be controlled.
Diabetes Symptoms Contributing to Poor Sleep
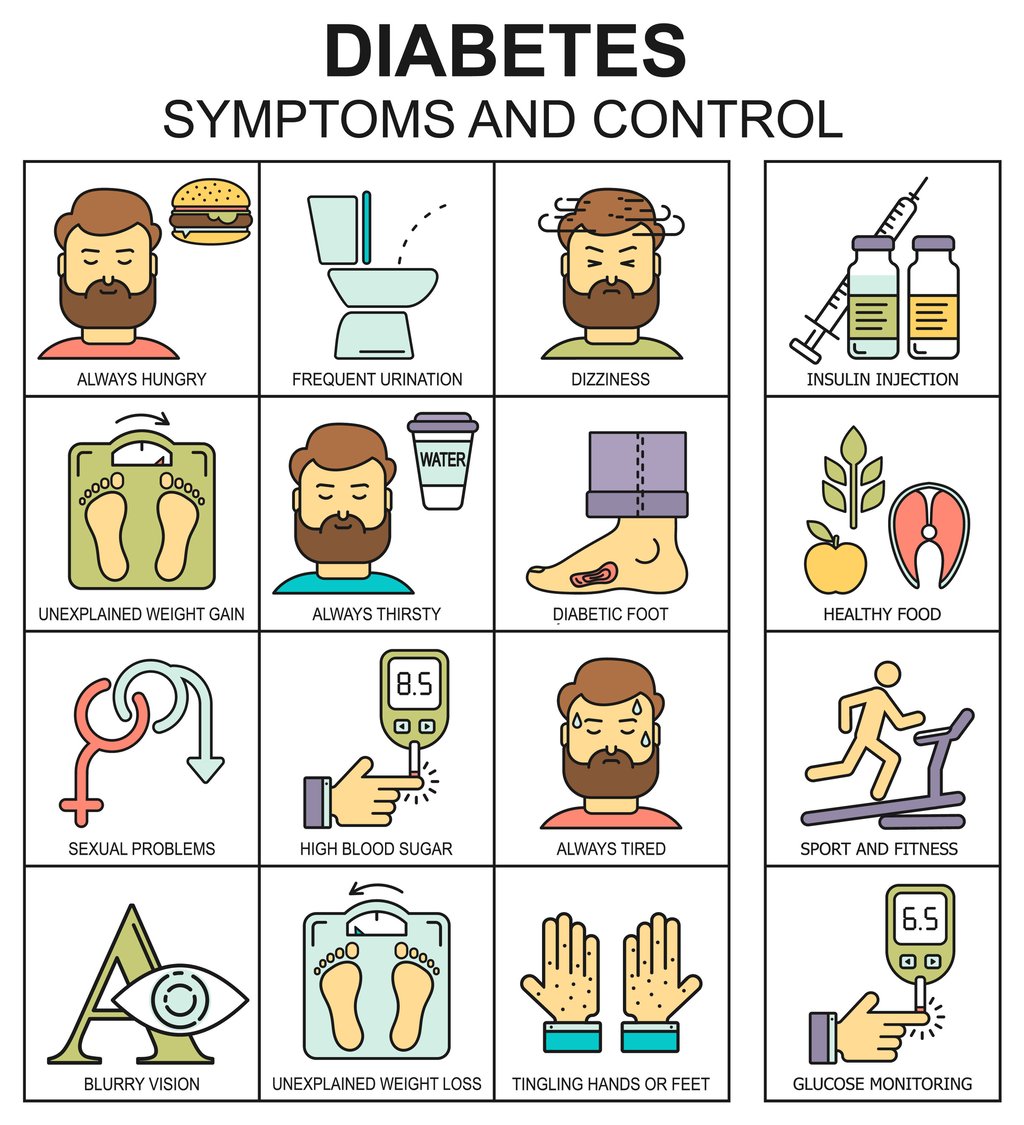
There are particular diabetes symptoms that can cause you problems when you are trying to sleep. These problems may include:
-
Frequent urination due to high levels of blood sugar.
-
Dehydration causing you to get up and drink more water (or other liquids) due to the excess glucose drawing water from your tissues.
-
Feeling dizzy, shaky, and sweating, which affects your sleep caused by low blood sugar.
Your sleep won't necessarily be impacted by your diabetes. It really comes down to the symptoms of diabetes you’re experiencing and how you’re managing them.
But, scientists and doctors alike have known for years that poor sleep can affect the hormone levels of your body and its ability to metabolize and regulate glucose. Therefore, if you’re not getting enough sleep and are excessively sleepy, it could increase your risk of diabetes, particularly Type 2.
Your risk of certain sleep disorders — like sleep apnea or restless leg syndrome (RLS) — is increased when you have diabetes. With sleep apnea, while you’re sleeping, you may pause in breathing periodically. When this happens, it wakes you up and you then begin breathing normal again. This, however, affects your sleep.
With RLS, you’re constantly feeling like you need to move your legs, particularly in the night when trying to go to sleep. It's an odd sensation that disrupts your normal sleeping pattern. When you have high blood glucose levels, your risk of RLS is increased and the frequent interruptions it causes in your sleep can keep you from actually getting into the important REM stage of sleep which is needed to restore your body.
Glucose Intolerance Due to Poor Sleep
Glucose tolerance varies day-to-day, hour-by-hour, and during your different sleep stages. You need sleep to restore your body and mind, however, sleep also affects your hormonal and metabolic processes as well.
Your slow-wave sleep, meaning your deep sleep, also correlates with temporary hormonal, metabolic, and neurophysiologic changes. While this might sound complicated, what it really boils down to is that these three things can have an effect on the stability of your glucose. Because of this, when your deep sleep takes over during the night, you have a slower glucose metabolism. During the second half of your night, during your REM stage of sleep, the effects are actually reversed. This, in effect, increases your chances of waking up.
In a Sleep Heart Health Study with over 1,600 participants between the ages of 53 through 93 years old, it was shown that impaired glucose tolerance (IGT) was caused by sleep restriction. The average sleeping time during the study was about seven hours of sleep a night. Around 27 percent of the participants slept six hours or less a night. The study showed that a six hour or less sleep duration or above nine hours had a higher prevalence rate of impaired glucose intolerance.
With these types of glucose metabolism changes you go through while sleeping, it's not a surprise that if you get poorer quality or less sleep on a regular basis that may have an effect on your overall glucose homeostasis.
Sleep Apnea and Glucose Intolerance
The role of sleep apnea and glucose intolerance is significant. Recently, there's been increased 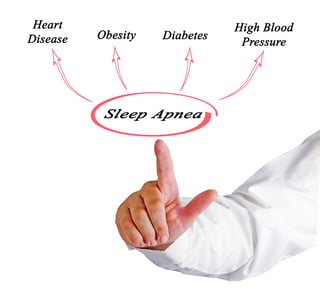 recognition that sleep apnea and other sleep-disordered breathing conditions can impact your glucose metabolism. The theory is that sleep apnea is linked with insulin resistance and glucose intolerance independently of other influences, such as your gender, age, body fat, and weight.
recognition that sleep apnea and other sleep-disordered breathing conditions can impact your glucose metabolism. The theory is that sleep apnea is linked with insulin resistance and glucose intolerance independently of other influences, such as your gender, age, body fat, and weight.
Glucose intolerance and obstructive sleep apnea (OSA) often co-exist because of the common obesity risk factor, but also independent of it as well. There was an up to 86 percent prevalence rate of OSA reported in diabetes patients, based on various criterions.
Sleep apnea can alter your diabetes management in a number of ways. For instance:
-
Your blood glucose levels can spike because of stress hormones being released.
-
Your body goes into the mode of fight-or-flight when you struggle for air.
-
When feeling tired, you probably won't take that lunchtime walk.
-
You may snack all day at work to stay awake.
When your sleep apnea is treated, it decreases insulin resistance, stabilizes your blood glucose levels, and improves your motivation and alertness. In fact, sleep apnea management is often used as a tool to control diabetes.
If you’re suffering with poor sleep, whether or not you think it's related to your diabetes, see your doctor. If your sleep is constantly disrupted and you don't get treatment, it can impact your daily functioning. You may have to alter your lifestyle a bit, which can make a huge difference.
In short, however, poor sleep or shortened sleep can ultimately increase your risk of developing diabetes and having diabetes and a disruption in your glucose can affect your sleep. Treatment for both can help.
If you are interested in learning more about the role of sleep and diabetes, click the image below to register for the Missouri Sleep 2017 Sleep Medicine Conference as Raymond E. Bourey, MD, will be speaking on Sleep and Diabetes.
